Introduction: Innovation Without Direction
AI algorithms in healthcare often match or exceed human experts’ performance across key diagnostic tasks. Yet as AI adoption across the healthcare industry accelerates, clarity on ways and goals to use AI in healthcare often lags. Pressured to “innovate with AI”, many healthcare organizations struggle to define clear objectives, use cases, or success metrics that apply to AI.
This gap between strategic intent and practical execution has become one of the most common barriers to meaningful AI implementation in healthcare. Without a proper understanding of its role in healthcare, AI risks becoming a buzzword rather than a transformative technology.
This article is for healthcare organizations seeking to clarify what AI in healthcare is, its role, and how to adopt it effectively.
Business Impact of AI in Healthcare
Driving efficiency gains, cost savings, and new revenue opportunities, the economic impact of AI investments in healthcare is becoming increasingly evident as healthcare is adopting AI across providers, payers, and technology companies 2.2x faster than other industries, according to the 2025: The State of AI in Healthcare.
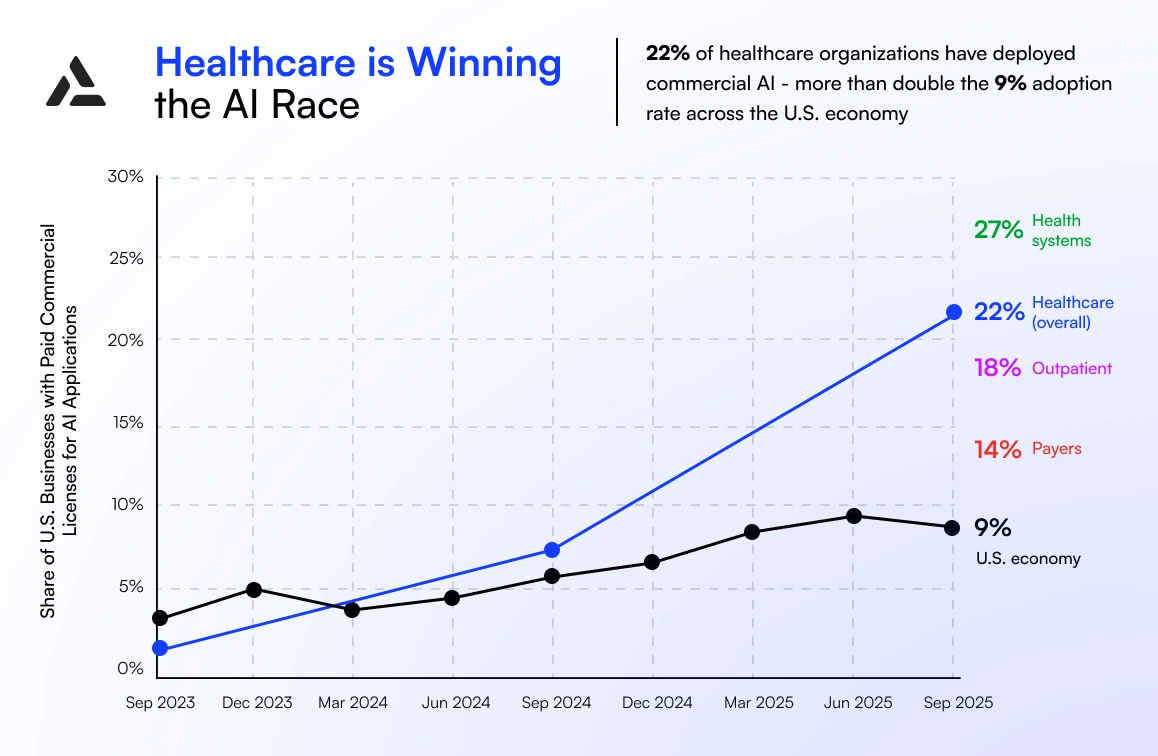
Total healthcare spending on AI in 2025 reached $1.4 billion, nearly three times the amount in 2024. Providers dominate AI adoption in healthcare, accounting for roughly 75% of total spend.
AI Investment and Market Growth
Healthcare organizations are actively allocating resources toward AI adoption, with a focus on measurable outcomes and return on investment.
Key trends include:
- Adoption trends: In 2024, 71% of US hospitals reported AI integration in their electronic health records (EHRs), up from 66% in 2023. Predictive AI models were most commonly used to predict inpatient health conditions or risks, while simplifying billing and facilitating scheduling were the fastest-growing AI functions.
- ROI considerations: The AI in healthcare market is poised for significant expansion — from roughly USD 36.96 billion in 2025 to over USD 613 billion by 2034 — indicating growing confidence in the long-term economic benefits of AI integration. In practice, healthcare organizations report measurable returns on investment, with leading systems seeing approximately $3.20 for every $1 invested and achieving payback in under 18 months.
Yet AI holds actionable cost-saving opportunities for both providers and payers. McKinsey reports that healthcare payers could see net savings of 13%–25% in administrative costs and 5%–11% in medical expenses by adopting existing AI and automation technologies, alongside potential revenue increases of 3%–12%.
What Is AI in Healthcare? Definition and Role
Using AI in healthcare involves using advanced algorithms and data-driven models to analyze medical and operational data, identify patterns, surface relevant insights, and support better clinical and operational decisions. The role of AI in the healthcare industry today is primarily decision support rather than a replacement for expertise.
Several global factors drive the rapid adoption of AI in the healthcare industry:
- Rising care costs: According to OECD Health at a Glance 2025, public spending on health will grow on average by 1.5% of GDP by 2045 across the Organization for Economic Co-operation and Development (38 member countries, including major economies such as the US, Japan, Germany, and the UK).
- Clinician shortages: Considering demographic shifts and rising care demand, the 2025 McKinsey Health Institute report projects a global shortage of at least 10 million healthcare workers by 2030.
- Growing availability of digital health data: Healthcare systems’ adoption of more data-driven solutions is the primary driver of the steady global digital health market’s growth, valued at approximately USD 420.08 billion in 2025 and projected to reach about USD 1,093.65 billion by 2034, according to a 2025 industry outlook.
- Advances in computing power and data infrastructure: McKinsey reports that the global race to build and scale compute infrastructure is one of the biggest drivers of technology investment. AI-ready infrastructure accounts for most of the data centers worldwide that need about $6.7 trillion in capital expenditures by 2030 to keep pace with compute demand.
Types of AI Technology Used in Healthcare
To address challenging clinical and operational needs, modern AI in healthcare leverages specialized systems that run a range of models.
Machine Learning and Deep Learning Models
Machine learning and deep learning are the analytical core of many AI systems used in healthcare today. These models are designed to learn from:
- Structured data: Lab results, Vital signs, Clinical measurements
- Unstructured data: Medical images, Free-text clinical notes, Signals from wearables and devices
Unlike traditional software, which follows fixed, rule-based instructions, AI technology in healthcare, based on Machine Learning and Deep Learning, is designed to learn and improve over time as it processes more data, detecting subtle patterns and early signals that are difficult to identify at human speed.
Generative AI in Healthcare
Generative AI in healthcare focuses on creating, summarizing, and structuring information. Thus, it allows clinicians to focus more on patient interaction by reducing administrative burden and improving information flow across care teams.
Common examples of generative AI in healthcare include:
- Clinical documentation drafting;
- Medical content summary from patient records;
- Care planning support that organizes relevant clinical information.
AI Agents and Agentic AI in Healthcare
The next evolution stage of AI technology in healthcare is the rise of AI agents. These systems go beyond single-task automation by connecting data, tools, and processes within defined clinical and operational boundaries.
Roles of AI agents in healthcare:
- Directing autonomous tasks across systems
- Coordinating providers, platforms, and services
- Triggering alerts, follow-ups, or interventions through workflow automation.
How Is AI Used in Healthcare? Core Applications
AI insight-driven support is transforming a range of healthcare areas:
1. AI in Diagnosis and Clinical Decision Support to improve accuracy and focus on patient-centered care through:
- Medical imaging and pattern recognition to spot anomalies earlier than traditional methods;
- Risk stratification and early disease detection to identify patients at higher risk and enable timely interventions.
2. AI in Predictive Analytics and Population Health to move from reactive care to proactive and data-driven strategies, anticipate clinical needs, and manage the health of the population at large through:
- Forecasting disease progression for individual patients or groups;
- Supporting hospital resource planning and reducing readmission rates.
3. AI in Patient Engagement and Virtual Care to reduce administrative burdens, keep patients engaged, and extend care beyond hospital spaces through:
- Symptom checkers and triage support;
- Appointment scheduling and follow-ups;
- Patient guidance and education between visits.
Real-World AI in Healthcare Examples and Use Cases
AI in healthcare is a reality, with practical applications and measurable impact demonstrated by the following real-life examples and use cases.

AI in Cardiovascular and Preventive Care
Heart disease remains a leading cause of morbidity worldwide, while up to 40-60% of cardiovascular diseases have heritability origins, meaning that they can be predicted. AI use cases in healthcare for cardiovascular care include:
- Risk prediction using genetic and biometric data, combining blood pressure readings, ECGs, wearable data, and body scanning results;
- Identifying high-risk patients before symptoms appear, enabling timely intervention, and reducing hospital readmissions by 40–45%.
Example: Significant improvements in early diagnosis rates of cardiovascular diseases (heart failure, valve disease, arrhythmias) in primary care settings were demonstrated by the application of AI-powered stethoscopes.

AI in Medical Imaging and Eye Care
AI is improving the early detection of preventable eye conditions by:
- Analyzing standard eye images for subtle changes, not recognizable by simple observation;
- Enhancing screening programs, reducing clinician workload, and improving detection rates.
Example 1: 96.7 – 99.8% accuracy was achieved in identifying sight-threatening conditions from retinal images during large-scale evaluations by AI systems for diabetic eye disease in NHS screening programs.
Example 2: Altris AI is an AI Decision Support for retina scans analysis called OCT – Optical Coherence Tomography. The system detects, identifies, and tracks 70+ retina pathologies on OCT scans, including the most widespread, such as Age-Related Macular Degeneration, Diabetic Retinopathy, and Glaucoma. The system is used by 500+ eye care businesses globally.

AI in Telemedicine: Care Beyond Hospital Walls
AI in telehealth services supports a range of remote workflows, including:
- AI patient monitoring, where algorithms analyse incoming data to detect early signs of deterioration;
- AI virtual assistants in healthcare, which guide patients through symptom reporting, education, and follow-ups;
- Visual AI in telehealth that enables real-time analysis of images or video during remote consultations to support clinical assessment.
Example: Widely recognized as a key player in AI-integrated telehealth and telemedicine services, Teladoc Health’s expanded Virtual Sitter solution helps to address workforce constraints, increasing remote monitoring capacity by up to 25% per staff member.

AI in Metabolic Health and Chronic Disease Management
AI is also transforming chronic diseases and metabolic health management by:
- Weight management and body composition monitoring through wearable and body scan data;
- Verifying self-reported information and tracking fat and muscle changes to support GLP-1 prescription programs;
- Integrating lifestyle, nutrition, sleep, and activity data to provide a comprehensive view of metabolic health.
Example: Over 60% of adults in the UK are overweight or obese, and obesity related ill-health costs the National Health Service (NHS) around $10 billion annually. 3DLOOK body-scanning technology measures full-body composition, predicts weight, and validates self-reported data using just two smartphone photos, completing the whole process in under a minute. After integrating 3D body scanning in GLP-1 prescription workflows, clinicians reported a 25–30% mismatch between self-reported data and data retrieved from uploaded photos, while manual verification of this kind took 4–6 minutes per case.
Benefits of AI in Healthcare
- Earlier diagnosis and improved outcomes: Analyzing complex datasets enables AI to reduce diagnostic delays and helps to cure patients efficiently by detecting muted patterns and emerging health risks.
- Reduced clinician workload: Helping medical personnel to focus on high-value clinical decisions and preventing medical burnout due to overload by automating repetitive tasks (image analysis, data verification, and routine patient triage) through AI systems.
- Cost efficiency and scalability: Integrating AI-powered predictive analytics and insights is a scalable solution that requires no increase in staff or infrastructure to optimize hospital resource planning, reduce unnecessary tests, and prevent readmissions.
- Personalized patient care: AI expands medical care capacity beyond traditional hospital settings by integrating clinical, lifestyle, and genetic data, making it accessible for tailored treatment plans, remote monitoring, and telehealth consultations.
Example: Apixmed supports B2B digital health services through a set of data-driven workflows, including:
- Data integration and interoperability, where clinical, laboratory, genetic, and lifestyle data are standardized and connected via HL7® FHIR® and LOINC;
- Automated interpretation and reporting, transforming raw health data into structured, evidence-based insights for clinicians and patients;
- White-label engagement tools, enabling partners to deliver branded portals, personalized reports, and ongoing preventive programs at scale.
Risks, Governance, and Compliance of AI in Healthcare
Privacy, security, and PHI protection
AI integrated into medical care systems routinely processes highly sensitive personal health information (PHI), making compliance with data protection standards non-negotiable. Without strong governance, even well-designed systems can expose organizations to operational, reputational, and regulatory risk — one of the most frequently noted disadvantages of AI in healthcare. Essential aspects of alleviating ethical and privacy challenges in AI in healthcare include, but are not limited to, secure data storage, strict data access controls, and transparent data retention policies.
Bias, fairness, model drift, and monitoring
Unequal outcomes across patient populations may result from AI tools trained on incomplete or unrepresentative datasets. Also, changes in care patterns, population composition, or data quality may force AI models deployed in live clinical environments to drift. At the same time, managing broader ethical issues in AI in healthcare entails addressing bias and performance degradation more broadly. Continuous monitoring, validation, and retraining of the systems are the milestones of responsible deployment and accuracy, safety, and ongoing clinical relevance.
Clinical responsibility and human oversight
One of the most essential aspects of AI’s involvement across industries is responsibility distribution, and in healthcare, clinical responsibility is directly related to human life and health quality.
AI in the healthcare environment is not a replacement for professional decision-making, and AI functions are strictly limited to decision support. Managing the limitations of AI in healthcare and reinforcing trustworthiness among stakeholders are possible only through a human-in-the-loop approach.
The absolute consent is that diagnosis and treatment plans must remain with licensed clinicians while AI automation improves operational efficiency and provides insights retrieved from vast data processing.
Regulatory pathways and regional requirements
To reduce long-term risks and continuously deliver sustainable results and value, verification against regulatory and operational realities is also critical. Depending on the region, AI solutions under consideration must align with local approval, validation, and deployment standards, such as the FDA in the US, the CE marking in the EU, and the NHS frameworks in the UK.
Procurement and integration risks
EHR interoperability, workflow disruption, and vendor lock-in are other practical challenges organizations face during AI implementation in healthcare. Evaluating how solutions integrate with existing clinical and IT infrastructures, developing risk mitigation strategies, and creating contingency plans are crucial at this stage.

Discover how AI-powered body intelligence is reshaping GLP-1 programs, telehealth, and digital health, from accurate remote assessments to safer and more engaging patient journeys.
The Future of AI in Healthcare
The future of AI in healthcare is in a total transformation from reactive care to proactive data-driven health management:
- AI-driven preventive care: Advanced predictive algorithms will identify emerging health risks long before symptoms appear.
- Fully integrated virtual health systems: Patient data, obtained from continuous monitoring, AI-guided consultations, and automated follow-ups, will unify with the data from telehealth platforms and clinical decisions.
- Agentic and autonomous care models: Omnipresent implementation of the most sophisticated and task-oriented roles of AI models in healthcare for automation, care coordination, and routine treatment protocols management under clinician supervision.
Conclusion: How to Start Using AI in Healthcare
Getting started with AI in healthcare does not require a complete organizational transformation from healthcare providers. For starters, focusing on high-impact applications and gradually integrating AI into existing workflows is a sufficient approach.
Key steps:
- Be curious: Explore how AI is already being used across the healthcare industry.
- Start small: Identify one practical use case and pilot it to evaluate outcomes before scaling.
- Collaborate with experts: Partner with technology providers who understand both AI and healthcare to ensure solutions are clinically relevant and operationally feasible.
- Measure outcomes, not hype: Focus on tangible improvements in efficiency, patient experience, and clinical decision-making rather than theoretical potential.
- Stay human: Let clinicians continue to guide care and make critical decisions while AI handles data, analysis, and repetitive tasks.